


Adaptive Optics Scanning Laser Ophthalmoscope (AOSLO)
Principles Systems Movies & Pictures Publications
this research is supported by:



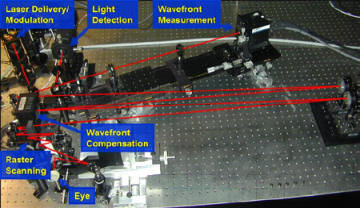
AOSLO operates much like a confocal microscopy, except that the eye is used as the objective lens and the living retina is the sample. Link here for an animation showing scanning/descanning of the AOSLO.
The principles of optical sectioning in the AOSLO are shown in the figures below.
|
Illumination: The illumination beam uses the eye's optics to focus the illumination light to a point on the retina. The scanning optics move the focused spot across the retina in a raster pattern. |
Detection: The confocal pinhole is conjugate to the plane of focus on the retina, so light that scatters from the plane of focus passes the through the pinhole and is detected by the photomultiplier. |
|
Blocking scattered light: Light that scatters from points deeper that the focal plane focus in front of the pinhole and are blocked by the confocal aperture. |
Blocking scattered light: Light that scatters from points that are in front of the focal plane focus beyond the pinhole and are blocked by the confocal aperture. |
The ability to reject light from outside the focal plane depends on how well you can focus light to a point using the optics of the eye. Hence, resolution in the SLO is limited by the aberrations of the eye. Adaptive optics are used to correct these ocular aberrations.
 |
 |
 |
|
AOSLOI:
Completed: 2001 at the University of Houston. Moved to Berkeley in January 2005. Deformable Mirror: 37 actuator Xinetics deformable mirror. Wavelengths: 840, 660 and 532 nm Features: patterned stimulus delivery, dual channel imaging |
AOSLOII:
Completed: 2005 at UC Berkeley. Deformable Mirror: 140 actuator MEMS mirror from Boston Micromachines Corp. Stroke 3.5 microns Wavelengths: 840 and 680 nm Features: compact design for clinical applications |
AOSLOIII:
Completed: 2010 in Dr. Jacque Duncan's lab at UCSF Deformable Mirror: 140 actuator MEMS mirror from Boston Micromachines Corp. Stroke 5 microns Wavelengths: 840 and 680 nm Features: Improved optical design and compact layout for clinical applications |
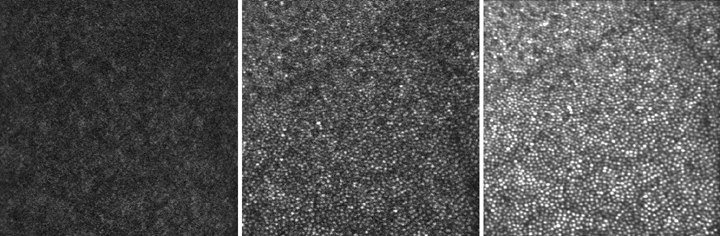
This figure shows the triple benefit of using AO in our SLO. The resolution, contrast and light throughput are all increased. The left image is taken after best correction of defocus and astigmatism, but not high order aberrations. The second frame is a single frame taken after AO correction. The third frame is a co-added set of 10 frames which have been corrected for distortions due to eye movements (see papers by Stevenson et al and Vogel et al). Virtually every cone is resolved in the registered frame. Image size is 1.2 degrees. Image location is about 1degree from the foveal center.
movie#1: AO on/off: (4.8 MB) This movie shows live imaging with and without AO. The magnitude of the aberrations is reduced by about 5 times by the AO. The movie shows that the overall amount of collected light is increased and that the contrast of the image is improved.
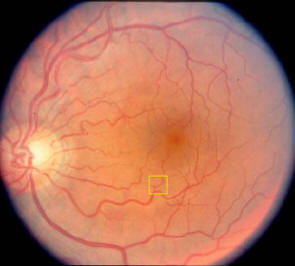
movie#2: Optical Sectioning of the Retina: (17 MB) The location of this video is about 4.5 degrees superior to the fovea. The yellow box on the image to the left indicates the location and approximate size of the video. In this video, we obtain confocal optical sections through the different layers of the retina, starting beyond the photoreceptors and moving through anterior retina. At first the photoreceptors are visible, followed by a blood vessel within which some evidence of blood flow can be seen. Then we resolve the nerve fibers overlying the vessel. The thickness of the retina at this point is about 300 micrometers from the nerves to the tips of the inner segments.
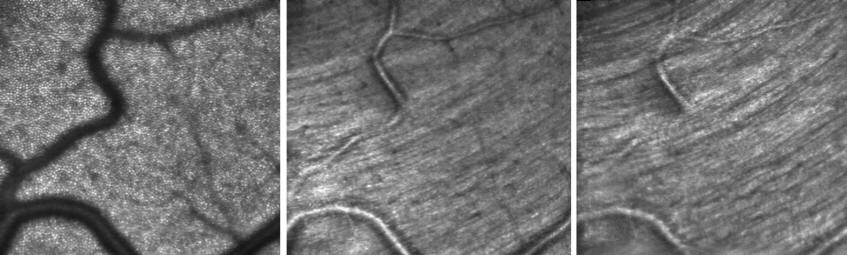
This figure show three optical sections through the retina. Left figure: cone photoreceptors; Center panel: blood vessels; Right panel: nerve fibers
movie#3: Blood Flow and Photoreceptors: (3.9 MB) This movie show white blood cells flowing through capillaries at the edge of the foveal avascular zone. The video is taken with green (532 nm) light. This video is stabilized offline using custom software (Stevenson et al., Vogel et al)
movie # 4: Stabilized video: (8 MB) This movie has been stabilized off-line using software developed by Scott Stevenson and colleagues at the University of Houston. The byproduct of the stabilization procedure is an excellent record of the retinal image movement. Accuracies are a fraction of a cone at frequencies up to 1 kHz.
movie #5: Stimulus delivery: (5 MB) By modulating the laser beam during the raster scan, it is possible to project complex images directly onto the human retina. Since the ingoing beam is pre-corrected by the AO system, the stimulus is projected with ultra-sharp clarity. The benefit of this method is that the delivered stimulus is automatically encoded onto the recorded video, allowing us to locate and track its position with an accuracy better than a single cone.
movie #6: Stabilized Stimulus Delivery: (2.9 MB) In collaboration with David Arathorn, Curt Vogel and Qiang Yang at Montana State University, we can estimate intraframe eye motion in real time during acquisition of AOSLO video. With this motion information it is possible to project a stimulus directly onto the retina and keep it locked onto a single cone. This video shows a sequence where a black cross stimulus is stabilized on a single cone in the retina (A white digital mark is also placed at the location of the stimulus).
NOTE: These videos have been compressed with Cinepak32. Even though they are 1/4 of their original size, they are still very large. There is also a slight degradation in these videos compared to their originals.
Acknowledgements
This work supported in part by by the National Institutes of Health (NIH EY13299 and NIH EY014365) the National Science Foundation Center for Adaptive Optics, managed by the University of California at Santa Cruz under cooperative agreement No. AST9876783, and Foundation Fighting Blindness.
Last update April 11, 2012